Abstract
INTRODUCTION
Allogenic stem cell transplantation (ASCT) is the only optimistic therapy for poor risk, relapse and/or refractory acute myeloid leukemia (AML) patients for better survival outcome. However, 40% of the patients relapse after ASCT translating into 2-year survival rates below 20% and majority of relapses occurs within 12-18 months of transplant (Devillier, Leukemia & Lymphoma 2013). Hence, it's reasonable to start maintenance therapy as early as possible for such high risk AML. Azacytidine, an hypomethylating agent (HMA) has been shown previously as a potential maintenance drug to be used in post transplant setting (Oran, Blood advances 2020). Recently Keruakous (Hematology/Oncology and Stem Cell Therapy, 2021) had showed that the relapse rate was significantly higher in the control cohort (66.67%) versus in the azacytidine maintenance cohort (25.81%). On the similar concept, we analyzed our AML patients who received maintenance with HMA post transplant.
OBJECTIVE
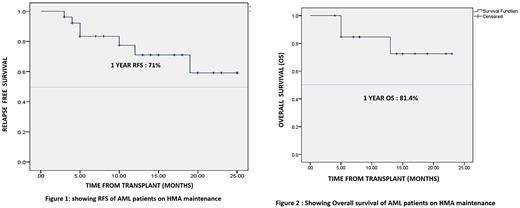
To analyze the Relapse free survival (RFS) and overall survival( OS) in AML patients post-transplant with the use of HMA maintenance therapy.
METHODS
It's a retrospective analysis of AML patients who have undergone ASCT at our centre between May 2020 and April 2022. Maintenance was given to all patients post ASCT irrespective of MRD status post transplant and risk classification pre-transplant. Patients who received maintenance with HMA (either azacytidine@ at 32 mg/m2 daily for 5 days 4 weekly or decitabine @10mg/m2/day for 5 days 6 weekly) and had completed at-least one cycle were included (Oran, Blood advances 2020 and Pusic, Biol of Blood Marrow Transplant 2015). Maintenance was planned for minimum of one year. OS and RFS was calculated by the Kaplan-Meier curves. Events included relapses and deaths.
RESULTS
Twenty-six patients (AML=24, MDS=1, CMML=1) received maintenance with HMA during the study period. Mean age was 31.5 (14-51) years and 15 (57.69%) patients were male. As per European Leukemia Net (ELN) 2017 classification 5 (19.2%), 12 (46.1%) and 7 (26.9%) patients were categorized into favorable risk, intermediate risk and adverse risk respectively. There were 14 (53.8%) patients in Complete remission (CR1) group, 10 (38.4%) in CR2 group and two(7.6%) were refractory disease. Source of graft was peripheral blood stem cell for all patients. Conditioning regimen was myelo-ablative in 22 (84.6%) patients, whereas 4 (15.3%) patients received reduced intensity. Donors were matched sibling (n=15, 57.69%), haplo-identical (n=6, 23.07%), matched unrelated (n=4, 15.38%) and mismatched unrelated(n=1,3.8%). Azacytidine was started within 100 days of transplant in 22(84.61%) patients. The median of number of cycles of HMA received were 6. The median duration of follow up was 13 months.
Seven (26.9%) patients completed 12 cycles. Acute Graft versus host disease (GVHD) was seen in 7 patients (26.9%) involving skin and liver whereas 3 (11.5%) patients had chronic GVHD involving skin and eye. Three (30%) patients developed GVHD prior and 7(70%) developed GVHD post initiation of maintenance. Six (85.7%) patients who relapsed on HMA maintenance had no prior acute or chronic GVHD. Out of all the 7(26.9%) patients who relapsed, 6 patients relapsed within a year and one patient relapsed after a year. One year RFS was 71% (Figure1), Event Free Survival was 67.9% and OS was 81.4% (Figure 2) Only 1 (3.8%) patient had Transplant Related Mortality (TRM), who died of COVID-19 infection. OS at 1 year for those in CR1 and CR2 was 84.6% and 88.9% respectively and it was not statistically significant (P = 0.95). There was no substantial hematological toxicity and resulting drug interruptions during the maintenance.
CONCLUSION
Early HMA maintenance seems to be an effective strategy post ASCT in AML patients to prevent early relapses and improving overall survival. Development of GVHD for patients on HMA had probably synergistic effect to prevent relapses by mediating graft versus leukemia effect without additional toxicity.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal